Post Vaccination/Regarding The Correct Assessment of Fatality Data From Covid-19 Cases During 2020
Determining The Fatality Ratios and Rates From Covid-19 Cases
An important characteristic of an infectious disease, particularly one caused by a novel pathogen like SARS-CoV-2, is its severity, the ultimate measure of which is its ability to cause death. Fatality rates help us understand the severity of a disease, identify at-risk populations, and evaluate quality of healthcare.
There are two measures used to assess the proportion of infected individuals with fatal outcomes. The first is infection fatality ratio (IFR), which estimates this proportion of deaths among all infected individuals. The second is case fatality ratio (CFR), which estimates this proportion of deaths among identified confirmed cases.
To measure IFR accurately, a complete picture of the number of infections of, and deaths caused by, the disease must be known. Consequently, at this early stage of the pandemic, most estimates of fatality ratios have been based on cases detected through surveillance and calculated using crude methods, giving rise to widely variable estimates of CFR by country – from less than 0.1% to over 25%.
For COVID-19, as for many infectious diseases, the true level of transmission is frequently underestimated because a substantial proportion of people with the infection are undetected either because they are asymptomatic or have only mild symptoms and thus typically fail to present at healthcare facilities. There may also be neglected or under-served segments of the population who are less likely to access healthcare or testing. Under-detection of cases may be exacerbated during an epidemic, when testing capacity may be limited and restricted to people with severe cases and priority risk groups (such as frontline healthcare workers, elderly people and people with comorbidities) . Cases may also be misdiagnosed and attributed to other diseases with similar clinical presentation, such as influenza.
Differences in mortality between groups of people and countries are important proxy indicators of relative risk of death that guide policy decisions regarding scarce medical resource allocation during the ongoing COVID-19 pandemic. This document is intended to help countries estimate CFR and, if possible, IFR, as appropriately and accurately as possible, while accounting for possible biases in their estimation.
A note on terminology:
The acronym CFR, as applied to the measure of the number of deaths among all persons with a disease, is most commonly referred to as the ‘case fatality rate,’ although strictly speaking this term is incorrect because the term ‘rate’ is used to denote a time component, which is absent in the CFR. Some authors have attempted to rectify this inconsistency by using the term case fatality proportion, or case fatality ratio, which is not bound by the numerator being a subset of the denominator (i.e., the definition of a proportion). The term ‘case fatality risk,’ used more rarely, is only correct if the duration of the clinical illness is known. For the purposes of this document, we will use the term “case fatality ratio”.
The acronym CFR, as applied to the measure of the number of deaths among all persons with a disease, is most commonly referred to as the ‘case fatality rate,’ although strictly speaking this term is incorrect because the term ‘rate’ is used to denote a time component, which is absent in the CFR. Some authors have attempted to rectify this inconsistency by using the term case fatality proportion, or case fatality ratio, which is not bound by the numerator being a subset of the denominator (i.e., the definition of a proportion). The term ‘case fatality risk,’ used more rarely, is only correct if the duration of the clinical illness is known. For the purposes of this document, we will use the term “case fatality ratio”.
COVID-19 case and death definitions
Countries have varying approaches to COVID-19 case definitions. Consequently, the numerator and the denominator of any formula used to calculate fatality rate will vary according to how they are defined. WHO recommends using the surveillance case definitions which are available in the WHO interim guidance on Global surveillance for COVID-19.
A COVID-19 death is defined for surveillance purposes as a death resulting from a clinically compatible illness in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID-19 disease (e.g. trauma). There should be no period of complete recovery between the illness and death.
A COVID-19 death is defined for surveillance purposes as a death resulting from a clinically compatible illness in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID-19 disease (e.g. trauma). There should be no period of complete recovery between the illness and death.
Calculating IFR
The true severity of a disease can be described by the Infection Fatality Ratio: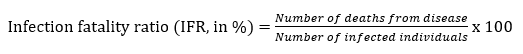 Serological testing of a representative random sample of the population to detect evidence of exposure to a pathogen is an important method to estimate the true number of infected individuals. Many such serological surveys are currently being undertaken worldwide, and some have thus far suggested substantial under-ascertainment of cases, with estimates of IFR converging at approximately 0.5 - 1%.
Serological testing of a representative random sample of the population to detect evidence of exposure to a pathogen is an important method to estimate the true number of infected individuals. Many such serological surveys are currently being undertaken worldwide, and some have thus far suggested substantial under-ascertainment of cases, with estimates of IFR converging at approximately 0.5 - 1%.
The true severity of a disease can be described by the Infection Fatality Ratio:
 Serological testing of a representative random sample of the population to detect evidence of exposure to a pathogen is an important method to estimate the true number of infected individuals. Many such serological surveys are currently being undertaken worldwide, and some have thus far suggested substantial under-ascertainment of cases, with estimates of IFR converging at approximately 0.5 - 1%.
Serological testing of a representative random sample of the population to detect evidence of exposure to a pathogen is an important method to estimate the true number of infected individuals. Many such serological surveys are currently being undertaken worldwide, and some have thus far suggested substantial under-ascertainment of cases, with estimates of IFR converging at approximately 0.5 - 1%.As serological studies require an investment of time and resources, there are many situations in which they may not be conducted timely, or even at all. Nevertheless, it remains crucial to monitor trends in severity in real time. In such situations, estimates need to be made with routinely available surveillance data, which generally consist of time-series of cases and deaths reported in aggregate.
Calculating CFR
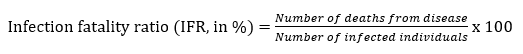
Case fatality ratio (CFR) is the proportion of individuals diagnosed with a disease who die from that disease and is therefore a measure of severity among detected cases:
 Reliable CFRs that can be used to assess the deadliness of an outbreak and evaluate any implemented public health measures are generally obtained at the end of an outbreak, after all cases have been resolved (affected individuals either died or recovered). However, this calculation may not hold in an ongoing epidemic, because it makes two assumptions:
Reliable CFRs that can be used to assess the deadliness of an outbreak and evaluate any implemented public health measures are generally obtained at the end of an outbreak, after all cases have been resolved (affected individuals either died or recovered). However, this calculation may not hold in an ongoing epidemic, because it makes two assumptions:Assumption 1: The likelihood of detecting cases and deaths is consistent over the course of the outbreak.
Early in an outbreak, surveillance tends to focus more on symptomatic patients who seek care, so milder and asymptomatic cases are less likely to be detected, leading to overestimation of CFR; this overestimation may decrease as testing and active case finding increase. One method to account for this is to remove from the analysis those cases that occurred before the establishment of robust surveillance, including application of clear case definitions (a method called left censoring).
Assumption 2: All detected cases have resolved (that is, reported cases have either recovered or died).
During an ongoing epidemic, some of the active cases already detected may subsequently die, leading to underestimation of CFR estimated before their death. This effect is accentuated in fast-growing epidemics (e.g. during the exponential growth phase of COVID-19).
Calculating CFR during an ongoing epidemic
CFR calculated using the above formula during ongoing epidemics provides a conditional, estimate of CFR and is influenced by lags in report dates for cases and deaths [13]. This leads to a wide variation in CFR estimates over the course of an epidemic, which tends toward a stable, final estimate of CFR as active cases are resolved.
One simple solution to mitigating the bias due to delays to case resolution during an ongoing outbreak is to restrict the analysis to resolved cases:

However, this method does not eliminate all biases related to delayed reporting. For example, differences in the time it takes for cases to resolve can bias this estimate. If people sick with the disease typically die quicker than they recover, CFR may be overestimated. If the reverse is true, it may be underestimated. Therefore, more sophisticated approaches that make use of statistical techniques to predict future outcomes among active cases based on the probabilities of past outcomes may be applied, including modified Kaplan-Meier survival analysis. Two important drawbacks to such approaches are first, that they tend to require individual-level data that are less accessible in real-time than aggregate case and death counts; and second, that they are less simple to do, generally requiring the application of advanced statistical methods.
Taking risk groups into account
The severity of COVID-19 has been widely reported to be influenced by age, sex and underlying comorbidities, and there is some evidence that other factors, such as ethnicity, are also independent risk factors. Any attempt to capture a single measure of fatality in a population will fail to account for the underlying heterogeneities between different risk groups, and the important bias that occurs due to their different distributions within and between populations. Therefore, efforts should be made to calculate risk-group-specific estimates of fatality risk in order to better describe the true patterns of fatality occurring in a population.
Potential bias in detection of cases and deaths
These biases may vary over the course of an outbreak:
- At the start of an outbreak, those cases detected are more likely to be severe or fatal. Patients with severe illness are more likely to present at health facilities and to be confirmed by laboratory test.
- Delays in reporting deaths can lead to underestimation of the CFR.
- COVID-19 cases and deaths occurring in the community that go undetected or are reported late because they were incorrectly attributed to other causes.
- If deaths are more likely to be reported than recoveries, an overestimation of CFR will occur. The reverse leads to underestimation.
Conclusion
In the COVID-19 pandemic, we have seen broad variations in naïve estimations of CFR that may be misleading. Countries are difficult to compare for a number of reasons. They may be more or less likely to detect and report all COVID-19 deaths. Furthermore, they may be using different case definitions and testing strategies or counting cases differently (for example, with mild cases not being tested or counted). Variations in CFR also may be explained in part by the way time lags are handled. Differing quality of care or interventions being introduced at different stages of the illness also may play a role. Finally, the profile of patients (for example their age, sex, ethnicity and underlying comorbidities) may vary between countries.
WHO

